01 Oct Blog: Joining efforts to complete seventeen MCDA’s
By Jan Erik Askildsen, University of Bergen
During the spring and summer months all partners have been intensively occupied with finalising their evaluations of 17 integrated chronic care programmes for persons with multi-morbidities, which is one of two deliverables from SELFIE work package 5.
The work builds closely on the former work packages, offering a multitude of methods and approaches for selecting and valuing key outcomes of integrated care. Persons with multiple chronic health problems often face limitations in many dimensions of life and they are disproportionally affected by the fragmentation in health and social care. In SELFIE we have therefore structured the outcome measurement according to the Triple aim, including improvement in ‘health and wellbeing’, ‘experience of care‘, and reduction in ‘costs of care’. Altogether, each integrated care programme is evaluated on a core set of eight generic outcomes and some further programme specific outcomes. This multi-dimensional framework can be analysed within the framework of a Multi Criterion Decision Analysis (MCDA). MCDA provides a novel and very relevant approach for evaluating programmes offering integrated care for persons with multiple chronic health problems leading to impairments in multiple life domains.
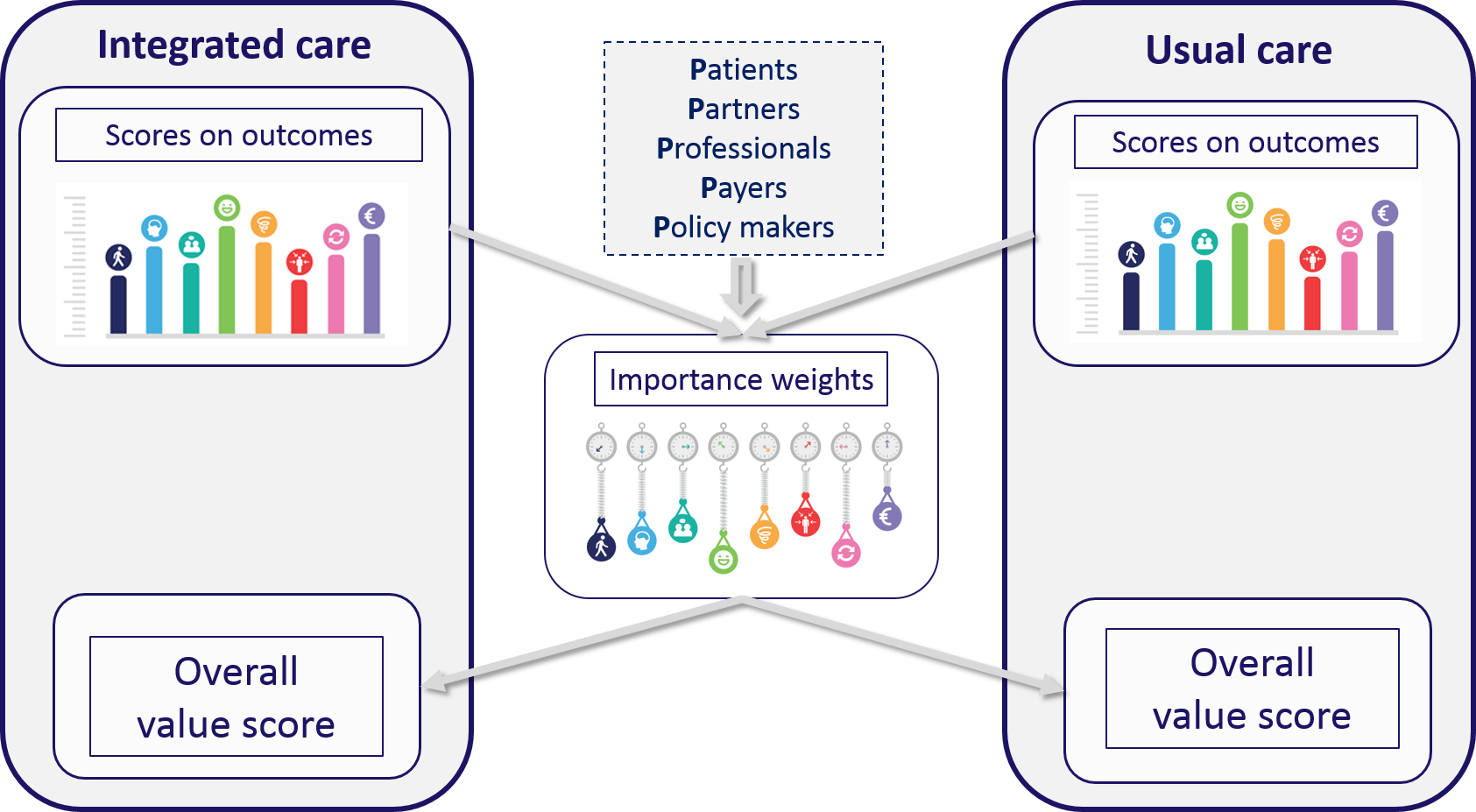
An MCDA is performed in several steps. Key elements of the MCDA are the measurement of the performance on the programmes on the outcomes in comparison to a control group, the elicitation of preference weights for these outcomes and the combination of the performance with the weights.
The SELFIE partners have measured the performance of the integrated care programmes using several different quasi-experimental research designs, like prospective controlled cohort studies, regression-discontinuity designs, difference-in-difference analyses. They have also made use of different data sources, including the SELFIE questionnaire that contains validated (domains of) instruments to measure the core set of outcomes and the programme-specific outcomes. These self-reported data were complemented with data collected from public registers and payers. Together with the EUR team we have prepared various guidance documents on for example propensity score matching, statistical analyses of panel data, MCDA calculations, cost calculations. Through a web-based survey in all countries to respondents representing 5 stakeholder groups (patients, partners and other informal caregivers, professionals, payers and policy makers), we are able to assess each group’s relative preferences for the different outcomes. Different revelation methods have been applied. The preferred approach is a Discrete Choice Experiment (DCE) but we also make use of a swing weighting approach. Interestingly, there is quite good correspondence among the different P’s in their preferences revelation, and among countries. Respondents give in general a high weight to ‘enjoyment of life’ and a low weight to ‘costs’, while patients seem to be relatively more concerned with ‘physical functioning’ than the other stakeholder groups. Another interesting finding is the relative high weight assigned to ‘continuity of care’ across stakeholders in Hungary and Croatia.
When evaluating each of the programmes, we assign weights to their performance on the outcomes to obtain partial value scores for the intervention and control groups. These are then summed to obtain the overall value score for both the intervention group and the control group. These scores are directly comparable between the two groups and the higher the total score the better outcome.
The data collection that the partners perform is comprehensive and very time consuming. Thus, for most of the 17 programmes, more data is still to be collected and further analyses are awaiting. Nevertheless, the preliminary results in general indicate moderate effects of the intervention, with a slight but not consistent tendency of the intervention group to perform better. For example, the Croatian palliative care programme had a higher value score than usual care, mainly due to higher partial value scores for Psychological Wellbeing and Person-centeredness, resulting from the combination of improvements in these outcomes and their relatively high weights.
Work package 5 is quite a challenging work package to lead and we try to support our partners in solving practical and analytical issues. Since data collection in ongoing, the EU has granted an extension of the delivery of WP5 until August 2019.
You can find the summary of the WP5 deliverable under Publications on this website.



No Comments